From MELD 26 to Sustained Recovery
Overview: The Arc of Recovery
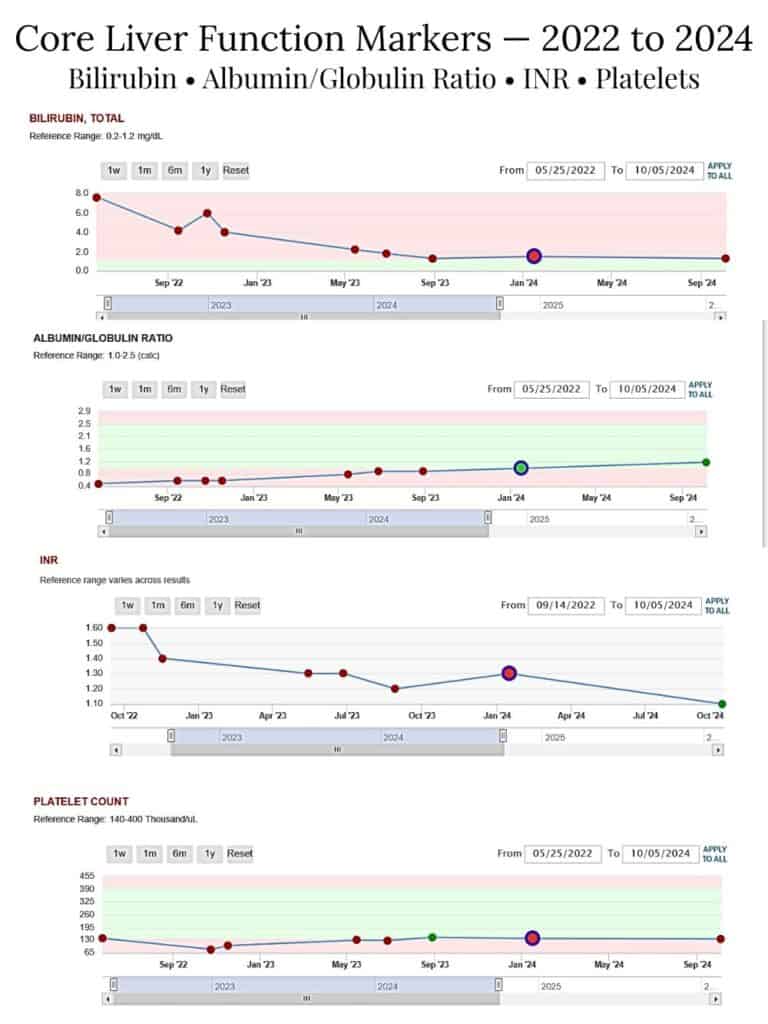
Scott’s bloodwork timeline documents his lab trends over time, from severe liver dysfunction to sustained recovery.
- Initial MELD score: 26
- Lowest documented MELD: 8 (with sodium)
- Primary timeframe covered: 2022–2024
- Current status: Sustained stability & Excellent Liver Function
Scott’s lab trends reflect a progression from severe liver dysfunction to restored synthetic function and long-term stability.
🔍 MELD Progression Snapshot
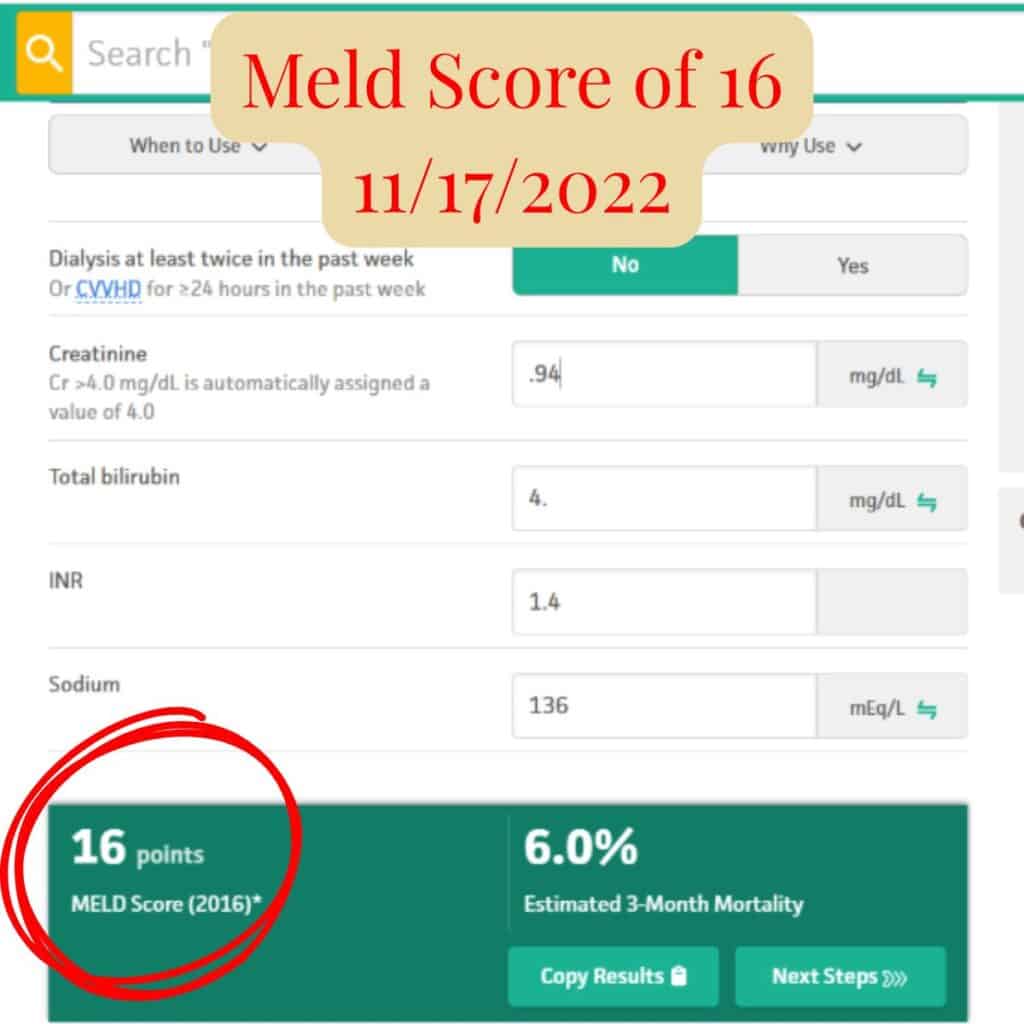
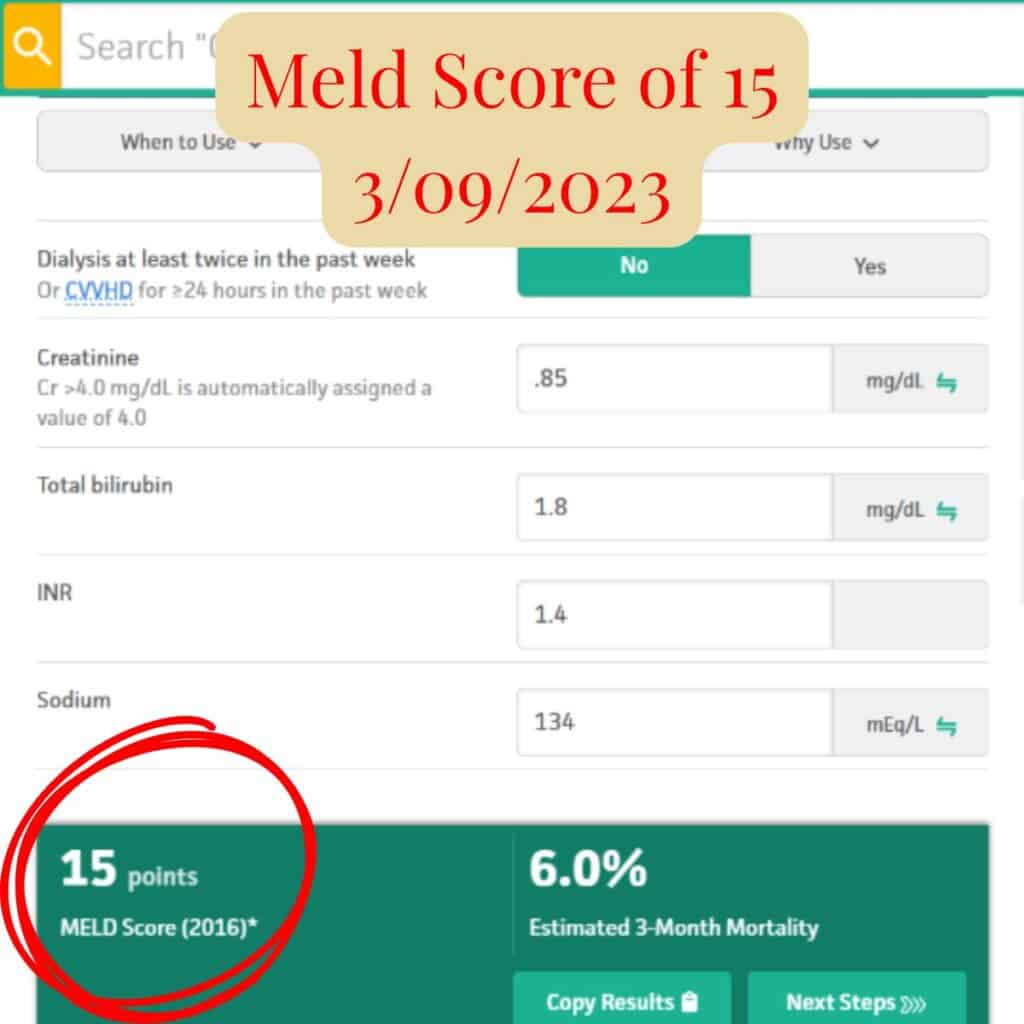
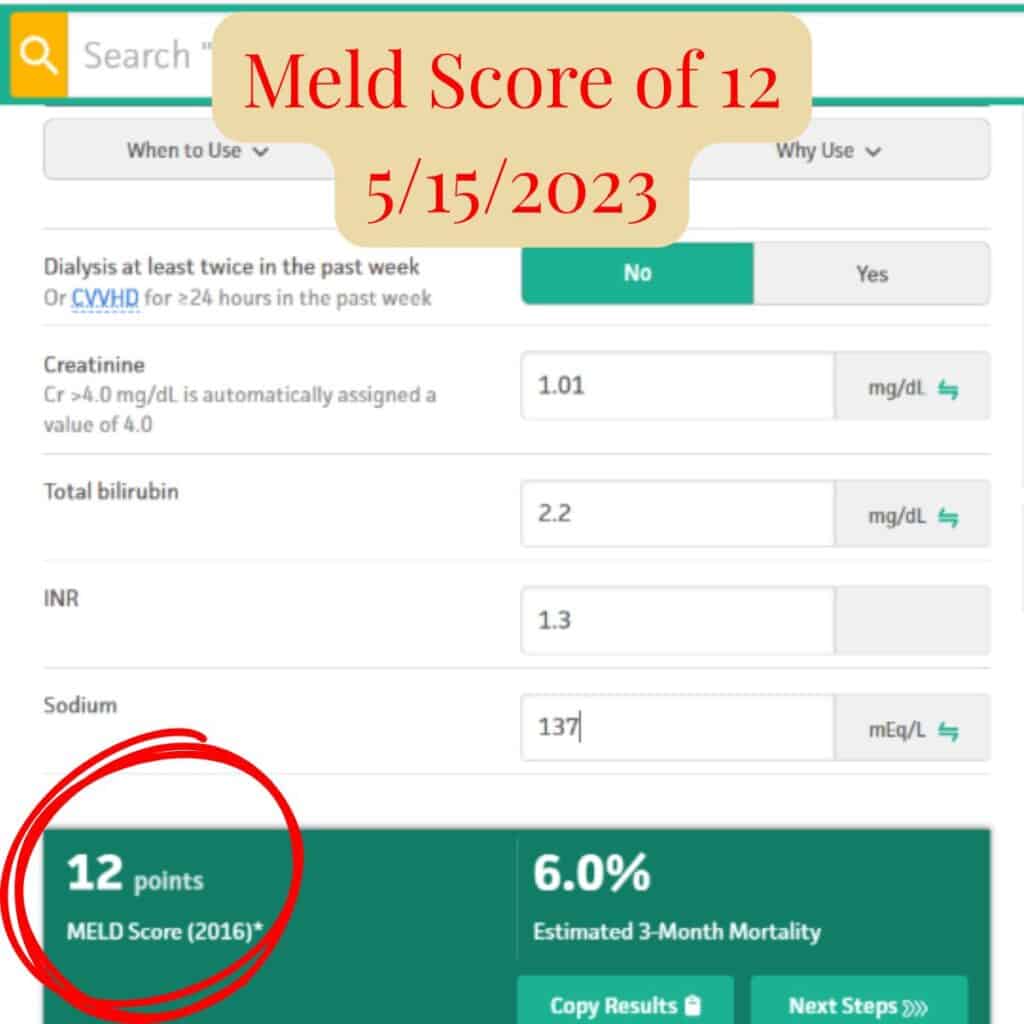
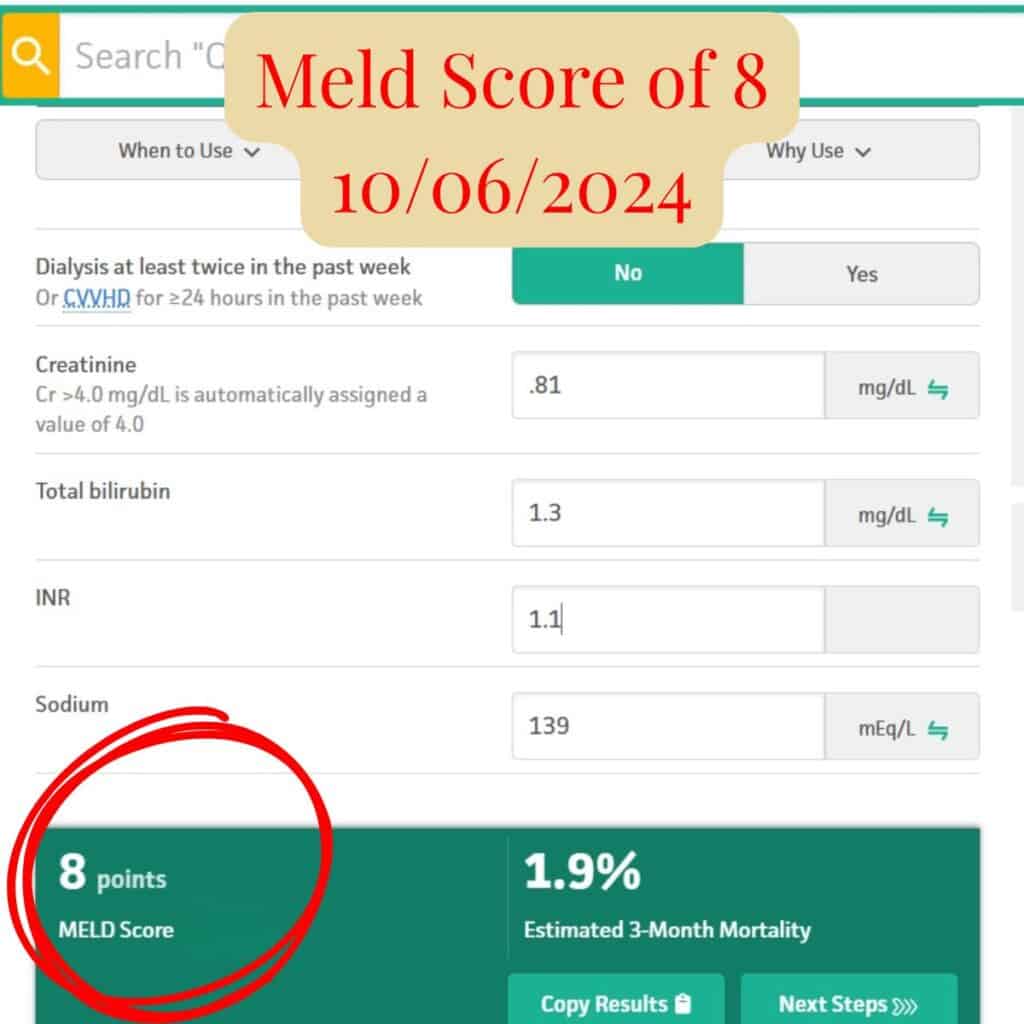
MELD scores over time reflecting improvement in liver function.
A MELD score of 8 reflects stable, well-compensated liver function; Scott’s transplant specialist described his liver function as excellent and no transplant needed.
Table of Contents
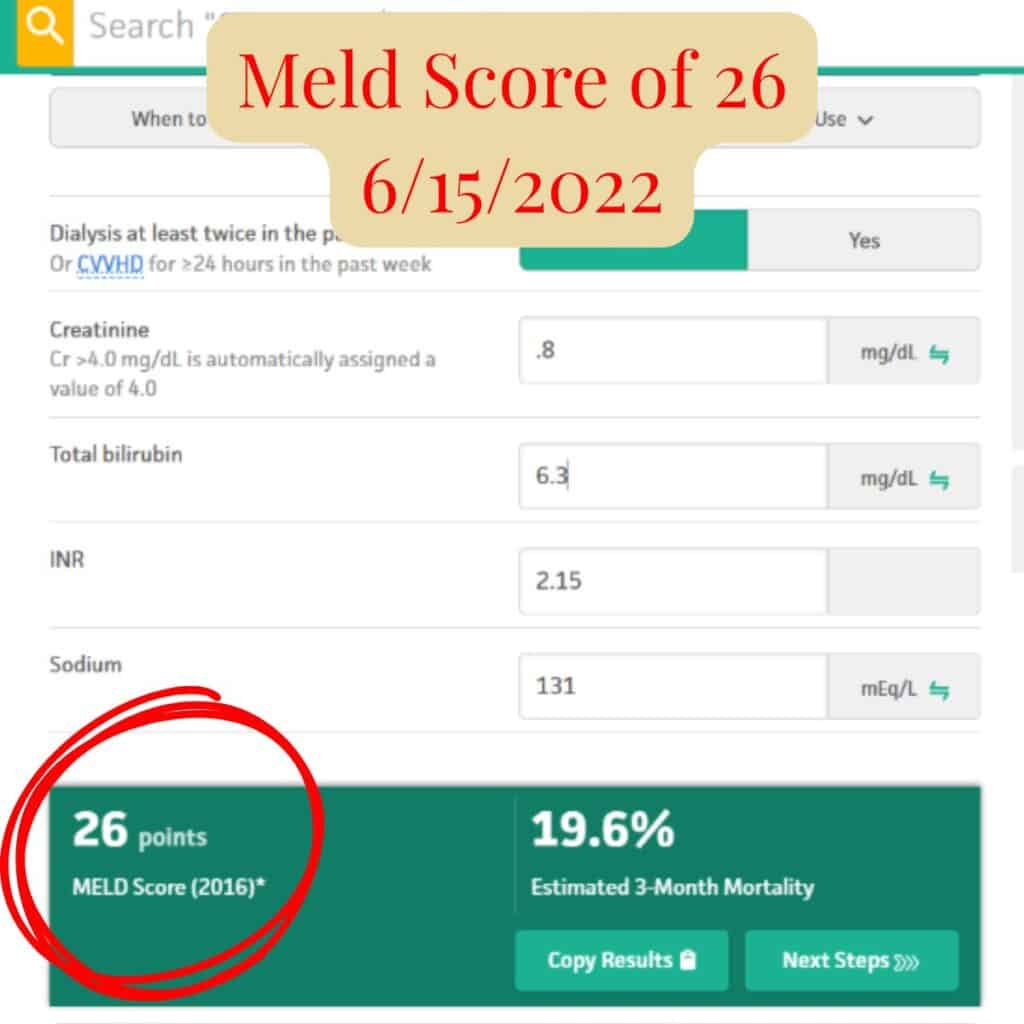
Phase 1: Diagnosis & Rapid Decline (2022)
This phase reflects advanced liver disease with significant functional impairment at the time of diagnosis.
Key laboratory findings
- Elevated bilirubin
- Elevated INR
- Low albumin
- Thrombocytopenia (low platelets)
- MELD score in the severe range
Note: INR values are missing for part of this timeline (May–September) because INR was not initially included in the standing lab order. When we realized INR is required to calculate MELD and track progress, we specifically requested it be added. Although we were initially told it wasn’t necessary to test that frequently, we explained that without INR we couldn’t calculate MELD or objectively measure improvement. The order was updated after that request — a reminder that you have to be your own advocate.
Interpretation
At this stage, labs reflected impaired liver function and poor prognosis. Transplant discussions were initiated, and symptoms consistent with liver failure were present.
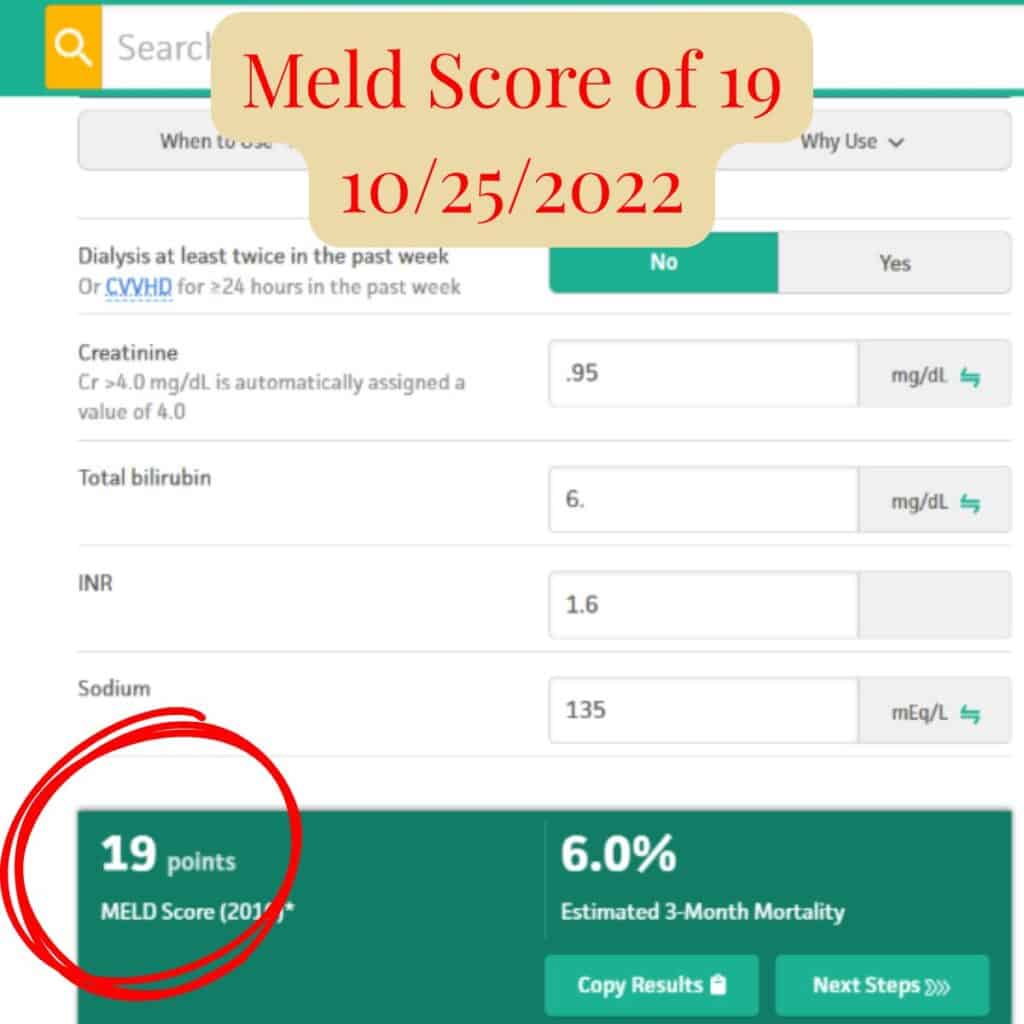
Rapid Improvement (June–November 2022)
Between June and November 2022, Scott’s MELD score dropped from 26 to 16 — a significant improvement over just five months.
During this period:
- No procedures were performed
- No transplant interventions occurred
- No phlebotomies had begun
The only changes were intentional and consistent:
- A fundamental shift in mindset
- Immediate lifestyle changes
- Food as a primary therapeutic tool
- Complete removal of gluten
- Targeted vitamins and supplements to support liver function
This phase marked the beginning of measurable recovery — before any later diagnoses or interventions — and demonstrated how quickly the body can respond when inflammation is reduced and the liver is given the support it needs.
Phase 2: Early Improvement & Stabilization (Late 2022 – Early 2023)
While Scott was being evaluated for transplant candidacy, lab trends began shifting and improving before he was ever formally listed.
Key laboratory changes
- MELD score decreased
- Albumin began improving
- Bilirubin and INR stabilized
- Platelet counts stopped declining
- Ascites appeared stable with no clear clinical worsening
Context note:
Educational materials often describe ascites as difficult to prevent or reverse in advanced liver disease. In Scott’s case, ascites resolved and diuretics are no longer prescribed — a change consistent with improved liver function and reduced portal pressure rather than temporary symptom management.
Interpretation
Although labs remained abnormal, trends began to matter more than individual values. These changes suggested the liver was responding to the food, lifestyle and supplement changes.
Phase 3: Sustained Recovery (2023–2024)
Context
Improvements held over time and became consistent.
Key laboratory findings
- MELD score continued to improve
- Albumin normalized
- Bilirubin and INR remained stable
- Kidney function remained normal
- Platelets improved and stabilized, though did not fully normalize
- Ascites resolved — medically confirmed diuretics no longer prescribed
Final Stable Labs (Late 2024)
- Albumin – within normal range
- Bilirubin – stable
- INR – stable
- Creatinine – normal
- Sodium – normal
- Platelets – stable
Interpretation
This phase reflects restored liver synthetic function and sustained stability. Platelet behavior during this period is consistent with recovery from advanced liver disease and does not indicate active decline.
Alpha-Fetoprotein (AFP)
AFP, a tumor marker monitored in chronic liver disease, remained within normal range throughout follow-up.
This provided additional reassurance during recovery.
Phase 4: Current Status (2025)
Context
Ongoing monitoring shows continued stability following recovery.
Key findings (summary)
- Liver function remains stable
- No recurrence of ascites
- No clinical signs of progression
- Mild laboratory fluctuations occurred at times and resolved
Imaging note: Recent imaging showed the liver to be mildly enlarged. The transplant specialist explained this can be consistent with hepatic/liver regeneration following resolution of inflammation and ongoing recovery, similar to how healthy liver tissue can regrow once injury/inflamation is removed.
Interpretation
Scott’s current lab profile reflects ongoing stability. Residual changes are consistent with adaptation after severe illness rather than ongoing disease.
About Platelets & Long-Term Recovery
Platelet counts improved and stabilized over time. While they did not fully normalize, this pattern is commonly seen after recovery from advanced liver disease and does not indicate ongoing deterioration.
In liver disease, platelets are often affected by prior portal hypertension and splenic sequestration. These changes may improve gradually or remain stable long-term, even when liver function is excellent.
Important Notes
- Lab values are shown as reported and interpreted in context.
- Trends over time are more meaningful than isolated results.
- This page documents one individual’s experience and is not medical advice.
- Medical decisions should always be made with a qualified healthcare provider.
Complete Laboratory Data
For readers who wish to review full laboratory panels, including CBC differentials and additional markers, complete data spreadsheet is available here:
[INSERT LINK TO COMPLETE LAB SPREADSHEET HERE]
How We Tracked the Numbers
By October 2022, as labs began coming in one report at a time — often spread across 30–50 page lab packets — it became difficult to see patterns clearly.
As Scott started feeling better, he created a simple spreadsheet to track each lab value side-by-side over time. This allowed us to compare trends much easier, not just isolated results.
We printed this spreadsheet and brought it to every transplant specialist appointment. The physician always asked if he could keep a copy, noting that it was far easier to review than the way the system compiled the data.
That spreadsheet became one of the most useful tools in understanding Scott’s recovery.
Want a Copy of the Spreadsheet?
If you’d like a copy of the spreadsheet we used to track Scott’s labs:
Download the bloodwork tracking spreadsheet we used and customize it for your own lab tracking.
You’re welcome to:
- use it for your own number tracking
- add or remove fields as needed
- use it to make sure you are getting all the tests to track at each blood draw
- adapt it to your own labs and timeline
This spreadsheet is for personal tracking and educational use only and is not intended to replace medical advice. Always review lab results with your healthcare provider.
Related Healing Journey Posts
- Scott’s Healing Journey — Part 1
- Scott’s Healing Journey — Part 2
- Scott’s Healing Journey — Part 3
- Scott’s Healing Journey — Part 4
A Note to Those Walking This Path
Recovery from liver disease is rarely linear. Some markers improve quickly. Others take time. Some never return to “never-happened” levels — and that does not mean healing failed.
What matters most is function, stability, and quality of life.
Healing can happen. 💛
For readers unfamiliar with how liver severity is commonly assessed, the MELD score (Model for End-Stage Liver Disease) is one of the standard tools used by transplant teams to evaluate liver function over time. You can learn more about how it’s calculated here.
✨If you’re new here, you might also enjoy 💖 Our Story, The Joy List 🌟— Our Ultimate All Day Playlist — the Recipes we lean on when food becomes part of healing — and 🐶 Fur Baby Tales, where we share life through Jack’s eyes.