The Diagnosis That Changed Everything
When nothing seemed wrong — until everything was.
Scott’s Healing Journey didn’t begin with symptoms or warning signs.
There were no warning signs telling us something was wrong.
For nearly the first eighteen years of our marriage, Scott didn’t get sick.
Not colds.
Not flus.
Not even the random things people our age start to complain about.
I was the one who got a cold most winters and a sinus infection every spring.
Scott was the one who just didn’t get sick — ever.
Later, a liver transplant specialist would explain something we didn’t know at the time — that iron overload from hemochromatosis can blunt normal illness signals, creating a kind of “super immunity” where damage can quietly build without obvious symptoms.
But back then?
None of that was on our radar.
The Year Everything Was Supposed to Change
By 2022, I was done.
We were in our mid-50s.
Scott was carrying about fifty extra pounds. I was carrying eighty to a hundred — which still feels surreal to say out loud.
I’d always been thin most of my life. Then, in my mid-to-late 40s, early menopause hit, cortisol went through the roof, and the weight came on fast — and refused to budge.
I didn’t want to just feel “fine for our age” anymore.
I wanted to feel good again.
I wanted to go low-carb.
Scott did not.
We’d tried it years earlier for a short stretch. He lost weight easily. I… did not. He found it boring. End of story.
Meanwhile, I was all in — and I really wanted him to do it with me. Not just for support, but because it’s a lot easier to cook when you’re eating the same way… and when pizza isn’t walking through the door on day twenty-two.
I’d already done a 21-day water fast — yes, really — and was planning a 40-day fast. It sounds insane, except after about four days you’re genuinely not hungry anymore. It’s the strangest thing. By week three, I actually thought, I could do this forever.
Then on day twenty-two, Scott came home with a pizza.
Game over.
I was not amused.
I’d been deep into research — low-carb, keto, carnivore — listening to Dr. Ken & Neisha Berry, and Dr. Boz learning how dramatically the body can heal when you stop fighting it with food. We’d spent years in the food and supplement industry ourselves. We knew the body could rebuild with proper nutrition.
We’d just taken it for granted.
So instead of fighting about diet, I suggested something else.
“Let’s just get a baseline,” I said.
“Bloodwork. Checkups. Let’s see where we actually are.”
Scott reluctantly agreed.
Table of Contents
The Appointment That Never Happened
Scott was scheduled first.
And that appointment never really happened.
The doctor looked at his bloodwork and immediately stopped everything. No exam. No routine next steps.
Instead, Scott was urgently referred to a liver transplant specialist.
At the time, we didn’t panic. We thought maybe it was a fluke. Or something fixable.
Looking back, Scott had been slowly gaining weight in the week or so before — and we assumed it was because we were indulging in all our favorite foods before “getting serious.”
Now we know it was likely early ascites.
It took about a week to get in with the transplant specialist. During that week, things escalated fast.
Scott began gaining fluid weight rapidly — sometimes five pounds in a single day. Within a short window, he’d put on an extra nearly forty pounds of fluid. He could barely walk. I was genuinely afraid he would go septic.
By that point, the “extra weight” conversation had completely flipped.
He now needed to lose closer to eighty pounds — at least forty of it fluid.
The First Liver Appointment
Before we even knew what questions to ask
This appointment was with a senior liver transplant specialist at a hospital within the Texas Medical Center in Houston — one of the leading transplant hubs in the country.
From the moment we walked in, the tone was unmistakable.
Because Scott drank beer — but almost never hard liquor — alcohol was immediately labeled the cause.
Other explanations weren’t considered.
Questions didn’t seem welcome.
There was no eye contact. He stared at the floor as he spoke.
No curiosity.
No sense that this was a puzzle to solve.
It felt like the conclusion had already been decided.
Then came the number that changed how we heard everything else:
MELD-Na score: 26
Because of that score, we were told Scott should be evaluated and listed for a liver transplant immediately.
At the time, we didn’t even know what that really meant — only that it carried weight, urgency, and finality.
And then we were told something far more definitive than a number.
Improvement was not possible.
I pushed back.
He was emphatic.
Not unlikely.
Not difficult.
Impossible.
We were told Scott had cirrhosis — and that cirrhosis meant there was no path to improvement, only decline. At best, lifestyle changes might slow progression.
Words like ascites, transplant, and die at any time came fast — explained bluntly, without space for discussion or hope.
Then came the sentence that stopped everything.
We were told Scott had less than a 50% chance of surviving two years without a transplant — and that he would die without one.
Period.
When the Room Went Quiet
Both of us describe that moment the same way afterward.
A blackout.
You hear the words, but your body shuts down. You’re no longer processing anything.
I pulled out my phone and started recording because I knew I wasn’t absorbing what was being said anymore. I knew I wouldn’t remember what came next.
Nothing after that sentence fully registered.
What We Asked For — and Were Refused
In the short time between the referral and that appointment, I’d been researching nonstop. I pulled Scott’s labs. I looked at patterns. I read everything I could.
One thing stood out.
I asked — and then begged — for a genetic test for hemochromatosis.
The doctor refused.
He said that wasn’t it.
Beer was the issue.
No test was ordered.
That refusal would matter far more than we understood at the time.
What we didn’t understand yet was that MELD wasn’t the only thing screaming for attention.
Scott’s bloodwork already showed extreme abnormalities — elevated ferritin and iron-related markers, liver enzymes that were badly out of range, and metabolic signals that didn’t fit the story we were being told — markers that pointed to metabolic dysfunction.
At the time, we didn’t know how to read those numbers.
We didn’t know what ferritin or iron saturation really meant.
We didn’t know how much damage they could quietly cause.
We just knew something didn’t add up.
The “Next Steps”
The plan we were given wasn’t about healing.
It was about eligibility.
Scott was put on two different diuretics, which worked quickly — though one came with unpleasant side effects, and the goal was always to get him off them as soon as possible. Within a few short weeks, he dropped nearly forty pounds of fluid.
We were told the next step was to test his other organs to see if he was healthy enough to survive a liver transplant and be placed on the list.
Ironically, the results were clear.
Every other organ tested strong and healthy.
Before we left, we were again told Scott had less than a 50% chance of surviving two years without a transplant — and that he could die at any time.
Not long after, we learned something else.
The estimated cost was around $1 million — and our insurance would not cover it.
The Decision We Didn’t Expect
We made the decision to change doctors.
What we didn’t know was how hard that would be.
Getting in with a new liver specialist took nearly seven months — a stretch of time that was both terrifying and, strangely, clarifying.
Because during that wait, we realized something important:
We couldn’t wait.
We couldn’t assume someone else would fix this.
And with no immediate medical path forward, doing nothing was not an option.
That window forced us to take responsibility for what we could control, with guidance and support outside the transplant system.
The Strange Part
The symptoms came after the diagnosis.
That’s what makes this story unusual — and important.
Scott wasn’t profoundly fatigued before the diagnosis.
The crushing exhaustion came about a week later.
Looking back, some of the weight we assumed was “just weight” was likely early ascites — something we didn’t understand yet.
The physical collapse followed the information, not the other way around.
That was the first moment we began to question how much belief, fear, and expectation might shape what comes next.
Why This Is Where the Story Starts
We’re typically very private people.
But we chose to share this because of what it changed — and what it made possible. At one point, I mentioned Scott’s turnaround in an online comment and was told it was impossible. That reaction is part of why we’re sharing the data.
This post isn’t about solutions yet.
It’s about documenting the true starting line.
Because what came next surprised everyone — including us.
In the posts that follow, we’ll share:
- Doctor opinions — good and bad
- Bloodwork results
- What changed, and how fast it changed
- And how Scott’s numbers — including his MELD score — improved in ways we were told were impossible
Why We’re Sharing This
Liver disease is being diagnosed at unprecedented rates, including in people who never expected it and in families facing it far too early. It’s no longer rare, and it’s no longer confined to one demographic. More people — including younger adults and children — are being diagnosed every year, often without symptoms until damage is already significant.
Increasingly, we’re also seeing links between liver disease and modern metabolic dysfunction.
We’re sharing Scott’s healing journey because what we found lacking wasn’t information — it was lived experience. Not fear-based warnings or isolated data points, but a clear, documented picture of what decline actually looks like, what recovery can look like, and what happens in between.
This series exists to show that full arc — from crisis to stability to recovery — using real labs, real timelines, and real life.
Hope without proof doesn’t hold for long. Proof without hope doesn’t help anyone heal.
This series exists at the intersection of both.
And this is where it begins.
Continue the story in Part 2: Impossible, They Said→
You can view Scott’s full bloodwork progression and MELD score changes here → Scott’s Bloodwork Timeline
✨If you’re new here, you might also enjoy 💖 Our Story, The Joy List 🌟— Our Ultimate All Day Playlist — the Recipes we lean on when food becomes part of healing — and 🐶 Fur Baby Tales, where we share life through Jack’s eyes.
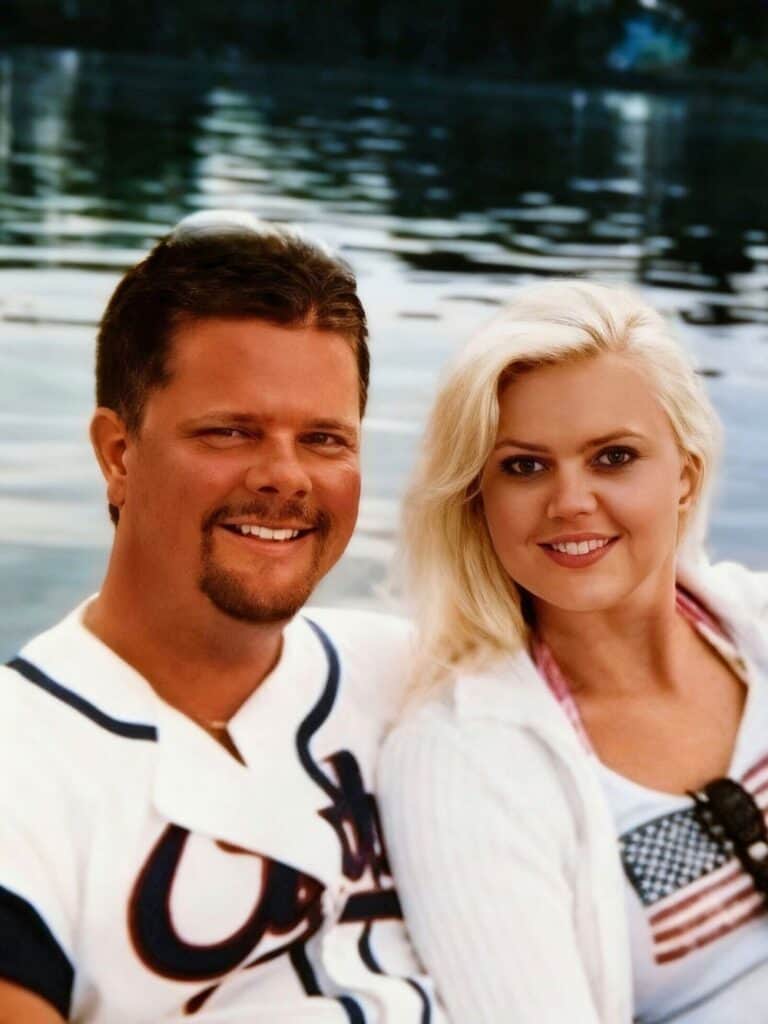
Meet Kristy, Scott & Fur Baby Jack

Recent Recipes
Recent Post
The Joy Is Contagious


